BD faces challenge in bridging healthcare gap
- Update Time : Friday, August 2, 2024

- Enhancing rural healthcare and reducing urban-rural disparities in Bangladesh
TDS Desk:
Bangladesh faces a significant challenge in bridging the gap between urban and rural healthcare. To improve it, we need a multi-pronged approach including increased government funding for rural health facilities, attracting and retaining qualified medical professionals through better incentives and living conditions, and utilizing innovative solutions like telemedicine to provide remote consultations with specialists. By focusing on these areas, Bangladesh can work towards a healthcare system that offers quality care regardless of location.
THE CURRENT URBAN FOCUS
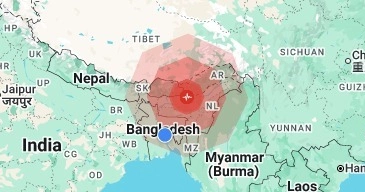
Rural areas in Bangladesh face significant challenges due to insufficient healthcare infrastructure. Many rural health facilities lack basic amenities, diagnostic tools, and medicines. According to the Bangladesh Bureau of Statistics (BBS), the national report of the country’s first digital “Population and Housing Census 2022” reveals that the total population stands at 169,828,911, with 68.34% residing in rural areas, while only 31.66% live in urban areas.
Despite this, a significant portion of healthcare resources is concentrated in urban centres, leading to delayed or inadequate treatment for rural populations and resulting in higher morbidity and mortality rates. The shortage of healthcare professionals in rural regions further exacerbates the problem. Many doctors, nurses, and specialists prefer working in urban areas due to better facilities, higher salaries, and improved living conditions. This urban-centric distribution of healthcare professionals leaves rural areas underserved and reliant on under-trained or untrained health workers.
Consequently, rural populations suffer from higher rates of preventable diseases and poorer health outcomes, highlighting the urgent need for targeted interventions to bridge these gaps.
THE DISPARITIES
The healthcare disparities between urban and rural areas in Bangladesh stem from a combination of factors, including infrastructure, workforce, accessibility, socioeconomic conditions, and technology. Urban areas boast superior healthcare infrastructure, with well-equipped hospitals and clinics, while rural regions often struggle with a lack of basic medical facilities and supplies.
The healthcare workforce is heavily skewed towards urban centres, leaving rural populations with insufficient medical professionals. Additionally, poor transportation infrastructure in rural areas hampers access to healthcare services, leading to delays in treatment and heightened health risks.
Socioeconomic factors further exacerbate these disparities, as higher poverty rates in rural areas limit residents’ ability to afford healthcare, and lower levels of education and awareness about health issues contribute to poor health outcomes.
Moreover, urban areas benefit from advanced medical technologies and digital health innovations, whereas rural regions lag due to limited internet connectivity and technological infrastructure, widening the gap in healthcare quality and access.
THE IMPACT ON COMMUNITIES
The healthcare disparities in rural Bangladesh, including the Chittagong Hill Tracts (CHT), profoundly impact communities, exacerbating existing socio-economic challenges. Inadequate prenatal and postnatal care contributes to higher maternal and infant mortality rates, reflecting a critical healthcare gap.
The prevalence of infectious diseases and chronic illnesses remains elevated due to delayed and insufficient treatment, compounded by limited access to preventive care and health education. These factors significantly burden rural economies, as untreated illnesses reduce productivity and perpetuate poverty cycles.
As a result, rural residents, including those in the CHT, often migrate to urban centres seeking better healthcare and living conditions. This migration strains urban healthcare resources and contributes to overpopulation, further highlighting the urgent need for targeted healthcare interventions and equitable resource distribution across rural areas, including marginalized regions like the CHT.
STRATEGIES FOR ENHANCING RURAL HEALTHCARE
Strengthening primary healthcare services through targeted investments in rural centres, coupled with the deployment of community health workers and mobile clinics, is essential. These initiatives not only relieve pressure on urban hospitals but also significantly improve healthcare access for remote and underserved communities.
Improving healthcare infrastructure across rural areas involves comprehensive efforts such as construction, renovation, and maintenance of healthcare facilities. Ensuring a consistent supply of essential medical equipment, medicines, and basic amenities like clean water and electricity is crucial to effectively meet healthcare needs in these regions.
Addressing the healthcare workforce shortage in rural Bangladesh, including the CHT, requires strategic interventions such as specialized training, scholarships, and incentives like rural practice bonuses to attract and retain healthcare professionals in underserved areas.
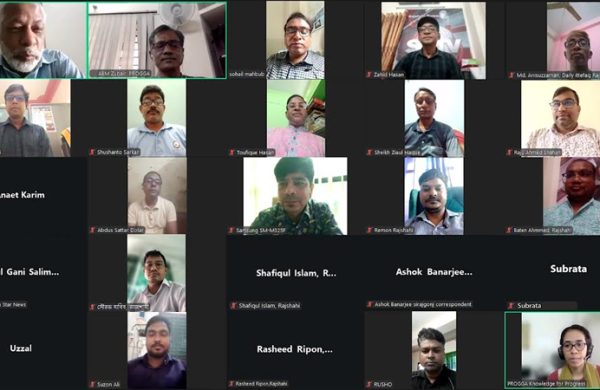
Technology integration, such as telemedicine and mobile health solutions, holds significant potential in bridging the urban-rural healthcare divide by enabling remote consultations, health education initiatives, and continuous patient monitoring.
Community engagement and health education efforts are pivotal in rural Bangladesh, including the CHT, to enhance awareness about preventive care, hygiene practices, and disease management.
Collaborative initiatives involving local communities and organizations play a crucial role in promoting healthier lifestyles and empowering communities to prioritize their health.
Government commitment and prioritization of rural healthcare, backed by adequate budget allocation and the implementation of comprehensive health insurance schemes, are essential for sustainable improvements. Effective governance and accountability mechanisms ensure efficient resource allocation and the successful implementation of healthcare initiatives that benefit all rural populations.
Bridging the urban-rural healthcare gap in Bangladesh is not only a matter of equity but also critical for the nation’s overall development. The stark disparities in healthcare access and quality hinder the country’s progress, underserving a significant portion of the population. Enhancing rural healthcare requires collaborative efforts from the government, healthcare providers, and the community, with targeted interventions addressing root causes and ensuring equitable healthcare access through policy prioritization, infrastructure development, and innovative healthcare delivery models.
In summary, a critical component of this strategy involves increasing the number of healthcare professionals in rural areas. This can be achieved by providing training and incentives such as scholarships, loan forgiveness programs, and rural practice bonuses, making rural postings more attractive to doctors, nurses, and specialists. Additionally, leveraging technology through telemedicine and mobile health (mHealth) solutions can significantly improve healthcare delivery in remote areas, facilitating remote consultations, health education, and continuous patient monitoring.
Community engagement and health education are also vital. Educating rural populations about health, hygiene, and disease prevention can lead to better health outcomes and reduced healthcare burdens. Community-based programs and partnerships with local organizations can play a significant role in promoting healthier lifestyles and raising awareness about critical health issues. Effective governance and accountability are crucial to ensuring the successful implementation of these strategies. The government must establish robust monitoring and evaluation mechanisms to track progress and address challenges promptly. By addressing the root causes of healthcare disparities and implementing strategic interventions, Bangladesh can pave the way for a healthier, more equitable future for all its citizens, ultimately contributing to the nation’s socio-economic development and prosperity.
A CALL TO ACTION
Bangladesh faces a critical imperative to bridge its urban-rural healthcare gap through unified action. Collaborative efforts among the government, healthcare professionals, non-governmental organizations (NGOs), and international partners are pivotal in executing comprehensive strategies. By prioritizing equitable healthcare, Bangladesh can ensure universal access to quality medical services across all regions.
Government leadership is essential, necessitating prioritization of rural healthcare in policy agendas with ample budget allocations and strategic health insurance schemes. Investments in upgrading rural healthcare infrastructure are crucial, alongside ensuring consistent availability of medical supplies and equipment. Incentivizing healthcare professionals to serve in rural areas through training, financial incentives, and conducive working environments is vital for mitigating workforce shortages.
The integration of technology, such as telemedicine and mobile health solutions, holds transformative potential in remote areas by enhancing access to consultations, medical advice, and patient monitoring. Simultaneously, community engagement initiatives focused on health education, disease prevention, and promoting healthy behaviours are essential. Collaborative efforts between local NGOs and community-based organizations can amplify these initiatives, fostering sustainable improvements in grassroots health outcomes. Effective governance and accountability mechanisms are indispensable for monitoring progress, addressing challenges promptly, and ensuring the success of interventions.
By fostering a united commitment to equitable healthcare, Bangladesh can chart a course toward a healthier, more resilient nation where every citizen, regardless of location, receives the healthcare they require and deserve for their well-being and prosperity.