We must reform the health sector to ensure equity
- Update Time : Tuesday, June 17, 2025

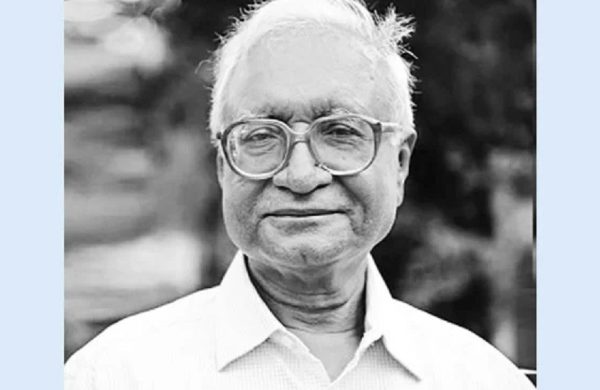
—Mamun Rashid—
In a small village in northern Bangladesh, a mother holds her sick child close, waiting for the only health worker who visits the area once a week. This is not just one family’s story but the daily struggle faced by thousands around the country. While Bangladesh has made progress in some health indicators, the ground reality tells a grim story. Especially in rural and low-income areas, people continue to suffer due to a lack of basic medical services. The system is burdened with limited funding, staff shortages, and services that fail to reach those who need them the most. If you are lucky enough, you get a doctor to write you a prescription, and most of the medicines you need will require spending money from your own pocket. If you are extraordinarily lucky, you might get some medicines from the hospitals, but they will likely be of low quality and at times may even be adulterated.
Despite so much talk about development in Bangladesh, healthcare remains one of the most neglected sectors. In the outgoing national budget, an allocation equivalent to only 0.74 percent of the country’s GDP has been set for public health. This is way below the five percent allocation recommended by WHO. As a result, most patients here are forced to pay out of their own pockets when they need treatment. In fact, in Bangladesh around 68.5 percent of all health spending comes directly from the patients—one of the highest rates in the world. For the poor, this often means choosing between medicine and food. Our health ministry is one of the top ones that don’t have a good track record of spending their budget allocation efficiently, not to mention the rampant corruption and malpractices contaminating its activities.
If someone living in an upazila or union falls ill, finding proper treatment can be a huge challenge. Union-level health and family welfare centres are supposed to provide basic care, but many are not functioning properly. The 2022 Bangladesh Health Facility Survey found that a significant number of public healthcare facilities across the country face severe shortages of trained staff, equipment, electricity, and medicines. These gaps have left large sections of our population without access to even the minimum healthcare support.
To address these long-standing problems, the Health Sector Reform Commission has made some serious recommendations. One of the core ideas is that primary healthcare should be recognised as a basic right under the constitution. This would mean providing free and essential health services to all citizens—whether they live in Dhaka or in a remote char area. If implemented, this move could bring real change to how healthcare is delivered across the country.
The commission has suggested forming an independent national health commission that would monitor reforms, ensure transparency, and make health governance more accountable. It also proposes setting up a separate and autonomous health service authority to improve professionalism and reduce political interference in the health sector. A dedicated public service commission for healthcare recruitment would ensure that only qualified and committed individuals are brought into the system. Moreover, multiple government agencies dealing with healthcare should be brought under one umbrella, specifically under the Directorate General of Health Services (DGHS), to reduce overlap and confusion.
Healthcare for women, especially in rural Bangladesh, has long been overlooked. The commission has recommended setting up a national institute for women’s health that would focus on issues like maternal care, safe childbirth, family planning, and diseases that particularly affect women. This is long overdue and would mark a significant step towards making healthcare more inclusive.
To decentralise healthcare, the commission recommends forming 11 regional health authorities at the divisional level. These bodies would take local-level decisions and speed up services. In cities, it proposes that primary healthcare centres be managed at the ward level, ensuring quicker access to services for urban poor communities who often fall through the cracks.
Another vital area is medicine. The current system allows pharmaceutical companies to influence doctors with gifts and incentives, pushing branded drugs over more affordable generics. The commission has rightly suggested banning such practices and encouraging doctors to prescribe using generic names. It has also proposed a nationwide pharmacy network that will make essential medicines available either free of cost or at subsidised rates, which could be a game changer for poor households.
Let’s also, with all due respect, talk about ensuring minimum possible governance structure and regulatory framework for prescribing and known-to-be-specialist doctors. There have been countless allegations that many of them have the tendency to prescribe more than required medicines to their patients, and more so rampantly recommending antibiotics without even recognising drug allergies and sensitivities. They allegedly don’t even ask the patients if they have an allergy or what medicine they have used previously for the identified problems. As many experts have pointed out, this can create havoc on the patients’ overall well-being, sometimes causing detrimental effects. Despite these dangerous practices, we seldom get to know any prescribing doctors being held to account. Many such specialists are also short on the communication to critical patients and/or their relatives. Medical communication is one important area where most doctors lack skill.
Implementing major ideas to improve our healthcare industry will no doubt not be easy. It will require political willingness, adequate funding, and sincere coordination among the ministries and agencies including rights bodies, may be the media as well. Health has never received the budget or more importantly the attention it truly deserves. That needs to change. The interim government now has a unique opportunity to start this transformation, and political parties engaged and to be engaged in this value chain should support these reforms for the benefit of the people.
The future of healthcare in Bangladesh depends on whether we can move beyond words and take real action. Whether someone lives in a high-rise building in Dhaka or a flood-prone village in Sirajganj, they deserve the same care and empathy when they fall sick. Overhauling our healthcare system is not just about building hospitals or appointing doctors. It is about fairness, compassion, and building a system that works for everyone with minimum possible responsibility. Only then can we say that our society truly cares for its ailing people.
——————————————————————————————-
Mamun Rashid, an economic analyst, is chairman at Financial Excellence Ltd and newly former managing partner at PwC Bangladesh. He was engaged with Bangladesh healthcare industry review and review of the health budget utilisation under the Sixth Five-Year Plan.